Overcoming stigma: Three strategies toward better mental health in the workplace
Overcoming stigma: Three strategies toward better mental health in the workplace
Courtesy of McKinsey & Company
By Erica Coe, Jenny Cordina, Kana Enomoto, and Nikhil Seshan
 (42).png)
The COVID-19 pandemic has taken a heavy toll on the global psyche. Today, as the world moves toward the end of the pandemic, almost one billion people have a mental-health or substance-use disorder—collectively referred to as behavioral-health conditions. As companies prepare for a postpandemic return to the workplace, identifying behavioral-health conditions and offering the necessary support for employees affected by them should be a top C-suite priority.
While most employers report that they are serious about employees’ mental health, many haven’t confronted one critical challenge: stigma. Using data from two recent US surveys conducted by McKinsey’s Center for Societal Benefit through Healthcare, this article takes a deep look at stigma in the workplace and its role in exacerbating behavioral-health conditions and driving down an employee’s self-worth and productivity. This is a widespread problem with serious implications. The good news is that employers are in a unique position to address stigma—especially during the short postpandemic window when many organizations are evolving their operations for the new reality of hybrid work.
Stigma and its impact
In behavioral health, “stigma” is defined as a level of shame, prejudice, or discrimination toward people with mental-health or substance-use conditions. Because of stigma, such conditions are often viewed and treated differently from other chronic conditions, despite being largely rooted in genetics and biology. Stigma affects everything from interpersonal interactions to social norms to organizational structures, including access to treatment and reimbursement for costs.
The National Academy of Medicine defines three primary forms of stigma, each of which can have far-reaching and harmful effects:
Self-stigma occurs when individuals internalize and accept negative stereotypes. It turns a “whole” person into someone who feels “broken.” As one employee told us, “Depression can be a terrible illness. It makes you feel worthless and without a purpose.”
Public stigma (which is sometimes referred to as social stigma) is the negative attitude of society toward a particular group of people. In the case of behavioral-health conditions, it creates an environment in which those with such conditions are discredited, feared, and isolated. As an employee explained, “There is such a stigma against mental-health disorders. But if you don’t talk about it, you suffer alone.”
Structural stigma (including workplace stigma) refers to system-level discrimination—such as cultural norms, institutional practices, and healthcare policies not at parity with other health conditions—that constrains resources and opportunities and therefore impairs well-being. “The number-one challenge I face is finding [healthcare] providers,” one employee told us. “It’s a problem for me, for my wife, and for my kids.”
The impact of stigma can be profound. At a time when people are at their most vulnerable and most in need of help, stigma prevents them from reaching out. This terrible paradox can deepen an illness that is often invisible to others. Evidence-based, effective treatments that allow people with behavioral-health conditions to live productive and fulfilling lives exist. Stigma creates a cloud of shame and uncertainty that obscures what could be a clear path to recovery.
Our analysis of our two surveys substantiates that impact. For example, many employees with a behavioral-health condition indicated that they would avoid treatment because they didn’t want people finding out about their mental illness (37 percent) or substance-use disorder (52 percent). Stigma was also associated with lower workforce productivity. Close to seven in ten respondents with high self-stigma levels reported missing at least a day of work because of burnout or stress.
Opportunity for employers to address stigma
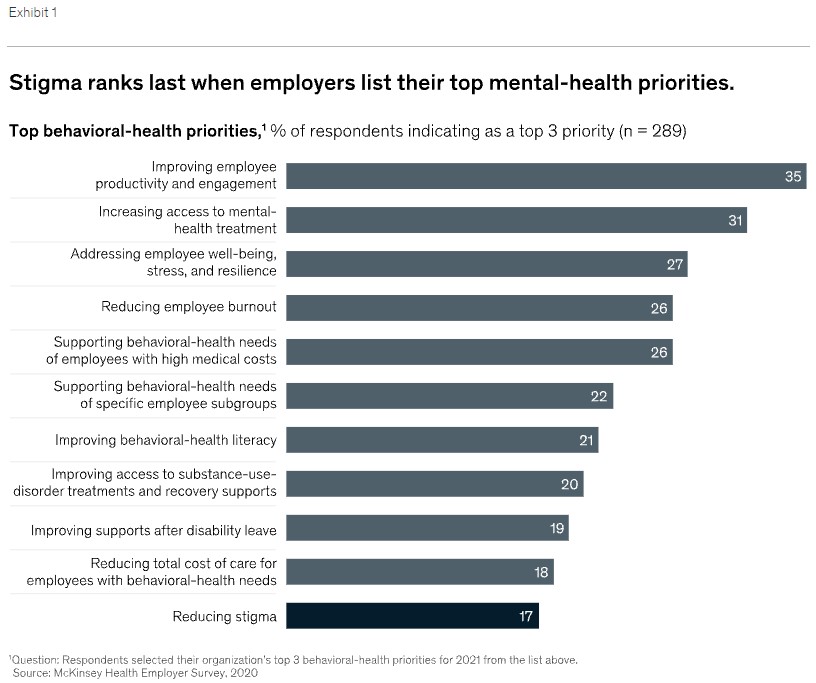
There is a pronounced disconnect between employer and employee perspectives on stigma in the workplace. While some 80 percent of the full-time-employed individuals we queried indicated that they believed that an antistigma or awareness campaign would be useful, only 23 percent of employers reported having implemented such a program. Further, when employers were asked to prioritize 11 potential behavioral-health-focused initiatives, they ranked stigma reduction last (Exhibit 1).
Yet 75 percent of the same employers acknowledged the presence of stigma in their workplaces. They know that their employees are afraid to speak up about behavioral-health needs. In fact, many leaders admit that they themselves may not be comfortable asking for help. So why aren’t they acting on what they know?
While companies may shy away from stigma because they imagine that it is too abstract to address, they are, in fact, missing an enormous opportunity. Employers can’t solve every aspect of substance-use disorders and mental illnesses in their workplaces. But stigma is something that they actually can change. Taking the right kind of actions can shift the dialogue from stigma to support.
The short window of time when organizations are evolving their operations for post-pandemic life is the perfect moment to act. Understanding, prioritizing, and planning for employees’ postpandemic mental health should be part of every company’s strategy for returning to the workplace. An inclusive culture and equitable benefits can lead to earlier, more effective intervention and support for people with behavioral-health conditions. Addressing stigma as a collective responsibility across three levels—organizational systems, leaders, and peers and teammates —will make those plans far more effective and help ensure the long-term health and commitment of the workforce.
To read the full article, please visit https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/overcoming-stigma-three-strategies-toward-better-mental-health-in-the-workplace
About the author(s)
Erica Coe is a partner in McKinsey’s Atlanta office and co-leads the Center for Societal Benefit through Healthcare; Jenny Cordina is a partner in the Detroit office and leads McKinsey’s Consumer Health Insights; Kana Enomoto is senior knowledge expert in the Washington, DC, office and co-leads the Center for Societal Benefit through Healthcare; and Nikhil Seshan is a consultant in the New York office and day-to-day lead of the Center for Societal Benefit through Healthcare.
The authors wish to thank Eric Bochtler, Ellen Coombe, Drew Goldstein, Brad Herbig, Tom Latkovic, Vidya Mahadevan, Etan Raskas, Bill Schaninger, and Jeris Stueland for their contributions to this article.
This article was edited by Rick Tetzeli, an executive editor in the New York office.
|